 Image 1 of 2
Image 1 of 2
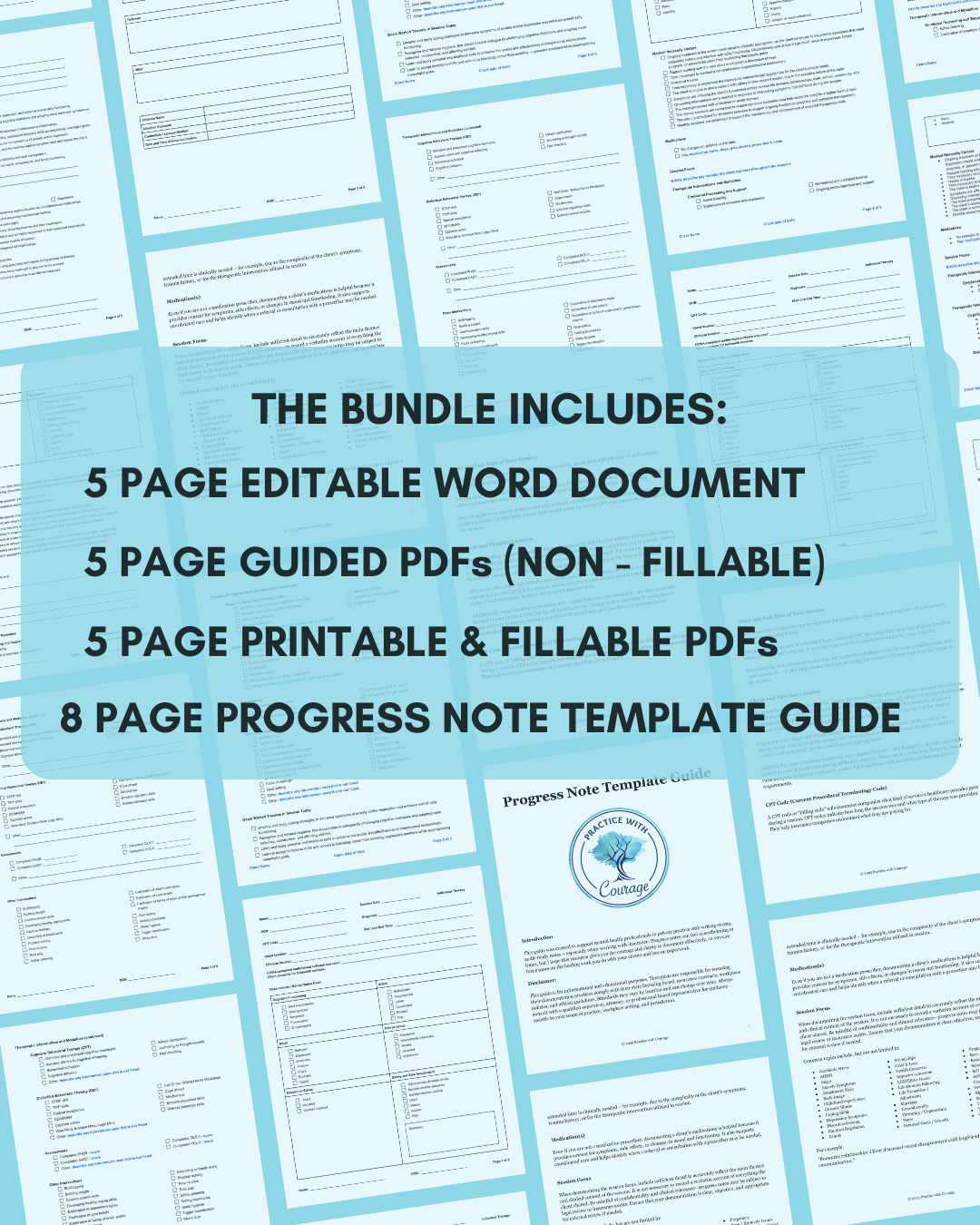 Image 2 of 2
Image 2 of 2
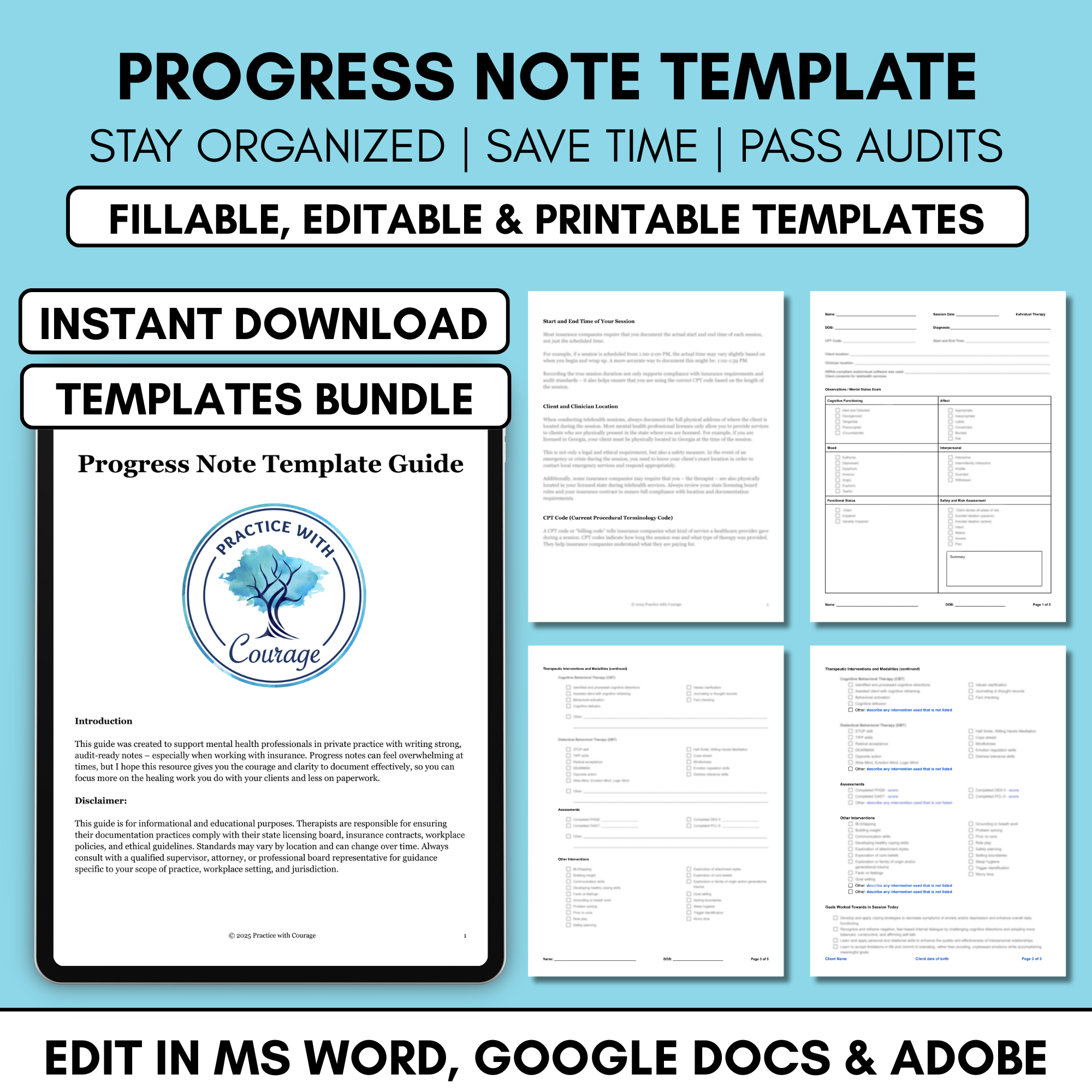
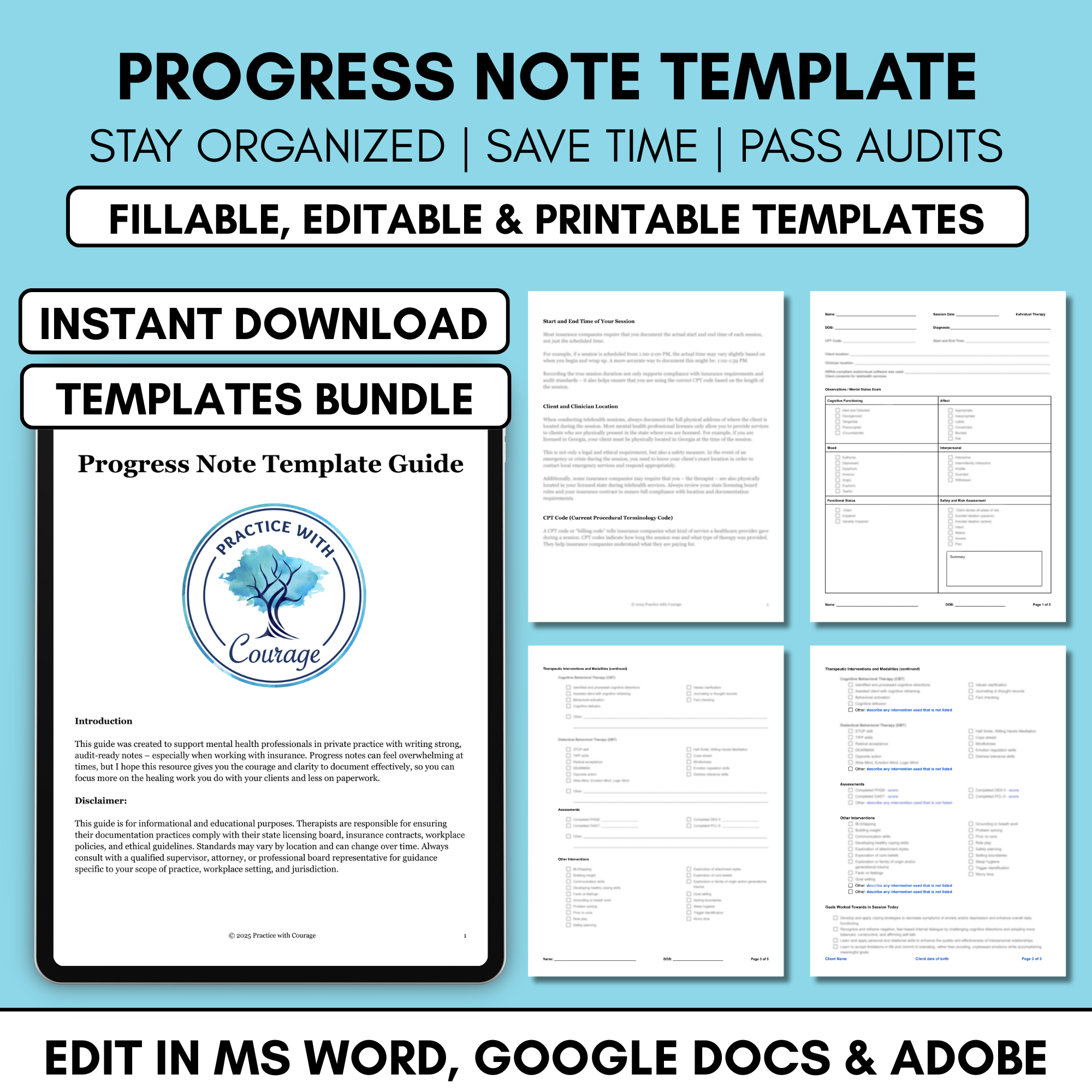
Editable Progress Note Template
Complete your clinical notes with confidence. This progress note template is designed for mental health professionals who want to document sessions clearly and efficiently. It helps ensure your notes include the key elements auditors look for while significantly reducing the time it takes to complete your documentation.
Created with private practice therapists (LCSWs, LPCs, LMFTs, psychologists, and other clinicians) in mind, this toolkit ensures your notes meet insurance and audit standards while cutting down the time it takes to complete them.
What's Included:
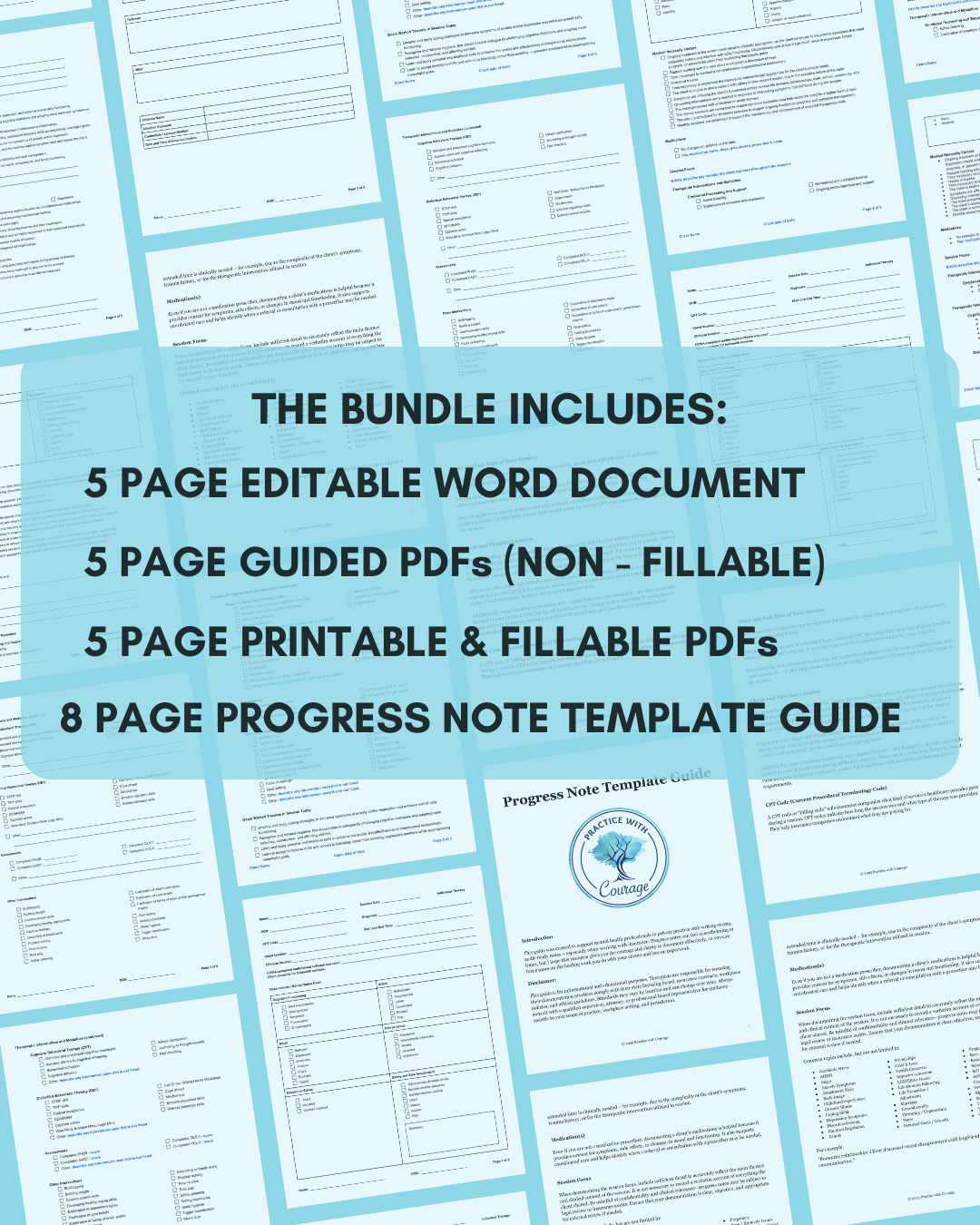
(1) Progress Note Template Guide: An 8-page guide offering tips for efficient clinical documentation. Covers topics such as session focus, diagnosing, CPT codes, how to document medical necessity, and more.
(2) Printable and Fillable PDFs: Two separate 5-page PDF templates – one for telehealth sessions and one for in-person sessions. Both PDFs are printable and fillable, offering flexible documentation options to suit your workflow. You can print them out and write directly on the provided lines during your sessions, or type into the fillable text fields and check off boxes for quick, paperless notes. Completed forms can be saved and uploaded directly to your EHR system.
(3) Editable Word Document: This is a single downloadable file that includes two 5-page progress note templates – one designed for telehealth sessions and one for in-person sessions. Customize this template to meet your specific documentation needs.
(4) Guided PDF (Non-fillable): This is a single downloadable file that includes two 5-page progress note templates – one for telehealth and one for in-person sessions. Descriptors written in blue guide you through what needs to be documented. Replace these with session-specific details for complete notes.
Why Therapists Love the Progress Note Template
Cuts note time in half
Keeps you audit-ready
Takes the guesswork out of documentation
Includes a guide that clearly breaks down what’s needed
A great alternative if you don’t want to use an AI note taker
Disclaimer:
This is a digital download. No physical product will be shipped.
Due to the nature of digital products, all sales are final.
You are responsible for ensuring your documentation meets the standards and requirements of your state licensing board, insurance payers, and workplace or practice policies. These standards may vary by location and setting, and are subject to change over time. Always consult with a qualified professional or supervisor in the state where you are licensed to ensure compliance.
The author is not liable for any consequences resulting from the use of this template, including but not limited to insurance clawbacks, denied claims, or incomplete documentation. By purchasing and using this product, you agree to assume full responsibility for how the content is adapted and used in your practice.
Complete your clinical notes with confidence. This progress note template is designed for mental health professionals who want to document sessions clearly and efficiently. It helps ensure your notes include the key elements auditors look for while significantly reducing the time it takes to complete your documentation.
Created with private practice therapists (LCSWs, LPCs, LMFTs, psychologists, and other clinicians) in mind, this toolkit ensures your notes meet insurance and audit standards while cutting down the time it takes to complete them.
What's Included:
(1) Progress Note Template Guide: An 8-page guide offering tips for efficient clinical documentation. Covers topics such as session focus, diagnosing, CPT codes, how to document medical necessity, and more.
(2) Printable and Fillable PDFs: Two separate 5-page PDF templates – one for telehealth sessions and one for in-person sessions. Both PDFs are printable and fillable, offering flexible documentation options to suit your workflow. You can print them out and write directly on the provided lines during your sessions, or type into the fillable text fields and check off boxes for quick, paperless notes. Completed forms can be saved and uploaded directly to your EHR system.
(3) Editable Word Document: This is a single downloadable file that includes two 5-page progress note templates – one designed for telehealth sessions and one for in-person sessions. Customize this template to meet your specific documentation needs.
(4) Guided PDF (Non-fillable): This is a single downloadable file that includes two 5-page progress note templates – one for telehealth and one for in-person sessions. Descriptors written in blue guide you through what needs to be documented. Replace these with session-specific details for complete notes.
Why Therapists Love the Progress Note Template
Cuts note time in half
Keeps you audit-ready
Takes the guesswork out of documentation
Includes a guide that clearly breaks down what’s needed
A great alternative if you don’t want to use an AI note taker
Disclaimer:
This is a digital download. No physical product will be shipped.
Due to the nature of digital products, all sales are final.
You are responsible for ensuring your documentation meets the standards and requirements of your state licensing board, insurance payers, and workplace or practice policies. These standards may vary by location and setting, and are subject to change over time. Always consult with a qualified professional or supervisor in the state where you are licensed to ensure compliance.
The author is not liable for any consequences resulting from the use of this template, including but not limited to insurance clawbacks, denied claims, or incomplete documentation. By purchasing and using this product, you agree to assume full responsibility for how the content is adapted and used in your practice.
